Drugs/Therapy
New Nanoparticle Technology for Breast, Brain Cancer Treatment
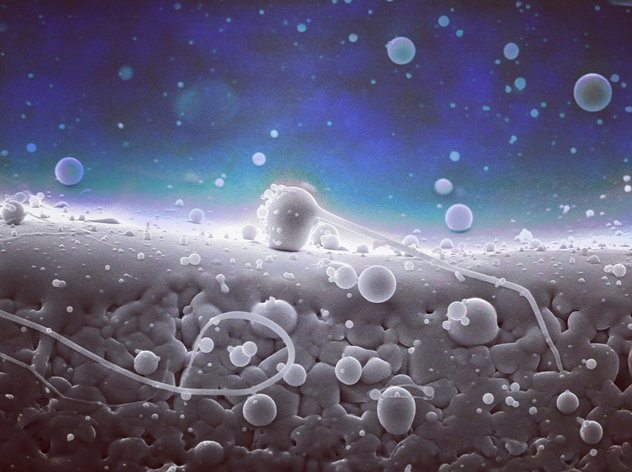
nanoparticles under electron microscope | (Photo : Muderkind/Wikimedia Commons)
Researchers at the Sylvester Comprehensive Cancer Center at the University of Miami Miller School of Medicine have unveiled a groundbreaking nanoparticle technology with promising implications for the treatment of breast cancer and brain metastases.
Led by Shanta Dhar, Ph.D., an associate professor of Biochemistry and Molecular Biology and assistant director of Technology and Innovation at Sylvester, the team's findings, published in the journal Proceedings of the National Academy of Sciences, highlight the potential of their innovative approach.
"I always say nanomedicine is the future, but of course we have already been in that future," said Dhar, referring to commercially available COVID-19 vaccines, which utilize nanoparticles in their formulation. "Nanomedicine is definitely also the future for cancer therapeutics."
The nanoparticle, designed to breach the blood-brain barrier, presents a multifaceted strategy to combat cancer. Loaded with two prodrugs targeting mitochondria, the energy production centers of cells, the nanoparticle demonstrated efficacy in shrinking breast and brain tumors in preclinical studies, Neuroscience News reported.
This novel approach addresses the challenges posed by brain metastases, secondary tumors that often arise from solid tumors like breast, lung, and colon cancer. By leveraging the unique metabolism of cancer cells, the nanoparticle's drug combination offers a targeted approach to disrupt tumor growth while minimizing harm to healthy tissues.
The team's method utilizes a biodegradable polymer nanoparticle coupled with two drugs developed in-house. One of these medications involves a modified iteration of the classic chemotherapy drug cisplatin, renowned for its ability to obliterate cancer cells by inflicting damage upon their DNA, thereby stalling their rapid proliferation.
However, cancer cells possess the capacity to mend their DNA, potentially fostering resistance to cisplatin. In response, Dhar's team engineered a modification, redirecting the drug's focus from nuclear DNA, which forms our chromosomes and genome, to mitochondrial DNA.
Mitochondria, the cellular powerhouses responsible for generating energy, harbor their own compact genomes-significantly lacking the DNA-repair apparatus found in larger genomes, a trait crucial for cancer therapeutic endeavors.
Recognizing cancer cells' adeptness at switching between diverse energy sources to fuel their relentless growth, the researchers combined their modified cisplatin, called Platin-M, with another drug they created, Mito-DCA. Platin-M interrupts a process in cancer cells that generates energy, while Mito-DCA targets a protein in mitochondria, slowing down another energy-making process called glycolysis.
Dhar expressed that creating a nanoparticle capable of reaching the brain was a lengthy process. Throughout her entire independent career, she has focused on nanoparticle research. During a previous project exploring various polymer types, researchers observed that a small fraction of these nanoparticles could penetrate the brain in preclinical trials.
Through further refinement of these polymers, Dhar's team succeeded in developing a nanoparticle able to cross both the blood-brain barrier and the outer membrane of mitochondria.
"We've encountered numerous challenges and successes along the way, and we're still delving into how exactly these particles traverse the blood-brain barrier," Dhar explained.
Subsequently, the team conducted preclinical trials with the specialized drug-loaded nanoparticle and discovered its efficacy in reducing both breast tumors and brain-seeded breast cancer cells, forming tumors therein. Moreover, this nanoparticle-drug combination showed minimal toxicity and significantly prolonged survival rates in laboratory experiments.
Moving forward, the team aims to refine their approach by simulating human brain metastases more accurately in the lab, potentially employing cancer cells sourced directly from patients. Additionally, they intend to evaluate the drug's effectiveness in laboratory models of glioblastoma, an aggressive form of brain cancer.









Join the Conversation